Assessment of the relative risk of antibiotic resistance associated
with the use of different classes of antibiotics; and with particular
antibiotics within classes
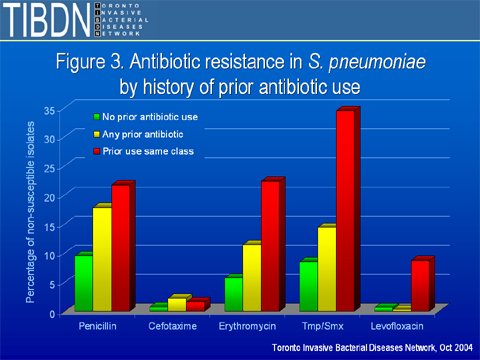
A recent history of antibiotic use increases the risk
of resistance in the infecting isolate, particularly within the
class of antibiotics (Figure 3). Prior receipt of any antibiotic
increases the chance that an infecting isolate will be resistant
to penicillins or cephalosporins. Prior use of macrolides, trimethroprim-sulfamethoxazole
or levofloxacin is associated primarily with a class-specific
effect: that is, a patient who has previously been given a macrolide
antibiotic is much more likely to have a macrolide resistant isolate,
than a patient who has received any other class of antibiotic.
Figure 3: Antibiotic resistance in S. pneumoniae by
history of prior antibiotic use
In Figures 4 and 5, the effects of different fluoroquinolones
are compared. Figure 4 shows the effect of the use of any flouroquinolone
on resistance to the different respiratory fluoroquinolones.
Figure 4: Rate of fluoroquinolone resistance in isolates from
patients who have and have not had prior therapy with any fluoroquinolone
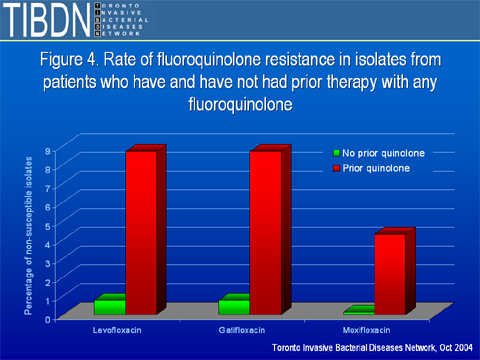
More than 95% of isolates from patients with a history of recent
fluoroquinolone use remain susceptible.
Figure 5: Rate of fluoroquinolone resistance in isolates from
patients who have and have not had prior therapy with the same
fluoroquinolone
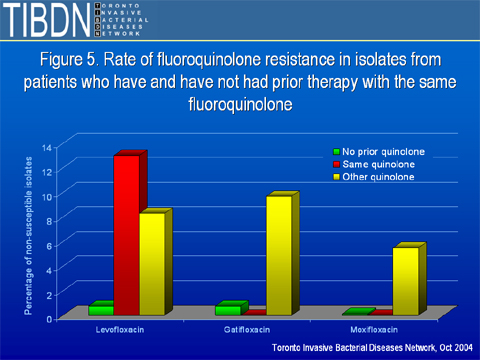
In Figure 5, resistance to individual fluoroquinolones is shown
based on which fluoroquinolone was used in the past. Thus, 0.77%
of isolates are resistant to levofloxacin if the patient had not
had fluoroquinolones in the past three months. In patients who
had been given a fluoroquinolone other than levofloxacin, 8.3%
of isolates were resistant. In patients who had received levofloxacin,
13% of isolates were resistant. The comparative figures for moxifloxacin
are 0.13% for patient who had not received a fluoroquinolone,
0.55% for patients who had received a quinolone other than moxifloxacin,
and 0 for patients who had received moxifloxacin. (Note that some
caution must be excercised here; numbers are currently limited
for moxifloxacin because of its recent licensure, and the difference
between 0.55% and 0 has not yet achieved statistical significance).
[Click here to access
PowerPoint file containing the above graphs.]



